| |
 |
| 

Sophia Cariati
Child Magazine, April 2001
|
 |
 |
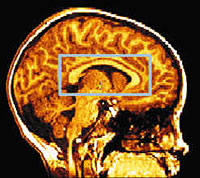
| Courtesy of Paul Thompson, PH.D., UCLA
Laboratory of Neuro Imaging. |
 |
Jordan Giedd, a healthy 5-year-old boy from Silver Spring, MD, climbs
onto a long, narrow table that fits snugly into the tubelike core of a
magnetic resonance imaging (MRI) machine -- a device used to examine
the inner workings of the body. His father, Jay Giedd, M.D., chief of
brain imaging at the Child Psychiatry Branch of the National Institute
of Mental Health (NIMH), and a technician, Michelle Williams, tuck
pillows behind his neck and slip a plastic ring around his head. After
reminding him to lie still, they slide the table into the tunnel so
Jordan's upper body is inside the core while his feet are visible
outside it. For about 30 minutes, he remains still as the machine
makes rhythmic, loud noises and captures three-dimensional photos of
his brain.
Over the course of five years, children like Jordan, who have normally
developing brains, and those with neurodevelopmental disorders such as
attention deficit hyperactivity disorder (ADHD), schizophrenia, and
bipolar disorder, visit NIMH in Bethesda, MD, to take part in
brain-imaging studies. These and hundreds of similar studies will
create the first atlas of the healthy, growing mind and help
researchers discover the basis for abnormalities.
"There is a big push for science to unlock the causes of
neurodevelopmental disorders so that we can prevent and treat them,"
says David Amaral, Ph.D., professor of psychiatry and neuroscience at
the University of California, Davis. "And MRI tests play an important
role in this process."
The MRI Experience
On a recent visit to NIMH, I watched as eight children ages 4
and older arrived at the hospital with their parents. NIMH is
one of seven centers across the U.S. compiling a database of
normal brain development by repeatedly scanning the brains of
400 healthy children ages 3 to 18. In tandem, NIMH researchers
use MRI to peer into the brains of hundreds of children with
ADHD, bipolar disorder (manic-depressive illness), and
childhood-onset schizophrenia. Most children will receive four
MRIs during the course of their involvement -- children ages 3
to 6 will come back every few months, while older children,
whose brains change less rapidly, return less frequently. Each
child is a paid volunteer, recruited through local newspapers
and community centers. The youngest children often come in
pajamas, close to their bedtime, with their teddy bears in tow.
Williams and Maureen Tobin, a research assistant, help the
children relax by telling them what to expect: "It doesn't hurt,
and there aren't any needles. But the machine is kind of loud,"
they explain. Unlike other imaging techniques, MRI is
noninvasive and doesn't involve radiation, so parents generally
feel comfortable allowing their children to participate. To help
the kids relax or, better yet, fall asleep, Mom or Dad sometimes
reads a favorite bedtime story. Once inside the machine,
children can see into the room through a mirror. Naturally, some
of them are frightened by the noise or feel claustrophobic, even
though their heads are outside of the machine. Though many are
at first apprehensive about lying in such a small, loud space,
Tobin estimates that less than 10% of all the children she sees
are too frightened to actually participate.
Unraveling the Mysteries of the Brain
Equipped with what are basically multimillion-dollar
oversized magnets, doctors can now use MRI to measure how
the brain changes as a child matures and learns. Doctors
can also see how brains respond when they perform specific
tasks like counting to 10. Until recently it was accepted
that most of brain maturation occurred in the first 18
months of life and that the process was complete by age 3,
but MRI studies are revolutionizing the way we think about
normal brain development. Experts now know that it
continues throughout childhood and well into early
adolescence.
Starting in 1987, Arthur Toga, Ph.D., professor of
neurology and director of the Laboratory of Neuro Imaging
at the University of California in Los Angeles, and his
colleagues repeatedly analyzed the brain scans of healthy
children ages 3 to 15 for up to four years. With the help
of computers, they tracked changes. In children ages 3 to
6, the area of the brain that helps learn new behaviors
and organize new skills underwent the most rapid growth.
"This shows how important it is to stimulate children at
these ages -- to play new games with them and to
strategize," says Dr. Toga.
Insights into Autism
Autism, which is believed to affect up to 1 in 500
children, impairs normal communication skills and
social inclinations. While most children can
instinctively read other people's minds through
facial expressions and body language, many with
autism are unable to use these social cues.
MRI studies implicate the amygdala -- a part of the
brain that controls social and emotional behavior --
in autism. Recently scientists at the University of
Cambridge in England studied the brains of people
with a mild form of autism and those of healthy
individuals while both groups attempted to interpret
facial expressions. The brain scans showed that the
amygdala was "turned on" in the brains of healthy
individuals during these exercises, while in the
autistic brains it remained dormant.
Researchers from the University of Washington School
of Medicine in Seattle found that this "social" area
of the brain was smaller in people with autism.
"Studies have found that there is something
functionally and structurally irregular in the
amygdala," says researcher Elizabeth Aylward, Ph.D.
Understanding ADHD
Although nearly one in every five children has
a neurodevelopmental disorder, scientists are
still unsure about what causes them and lack
conclusive tests for their diagnosis. But for
a condition such as ADHD, which affects 3% to
5% of children in this country, they're
uncovering helpful information.
For years experts have debated whether ADHD is
a real problem or a label too readily placed
on rambunctious, healthy children. Unlike
diabetes, a disease detected with a simple
blood test, ADHD is diagnosed by observing a
child's behavior. Parents, educators, and even
some doctors argue that this "fuzzy" technique
has led to an overdiagnosis of ADHD, resulting
in the overmedication of many children. But
brain-imaging studies are finally providing
proof that ADHD has a biological origin.
In 1996, F. Xavier Castellanos, M.D., chief of
the ADHD Research Unit at the child psychiatry
branch of NIMH, led a landmark MRI study that
compared the brains of boys diagnosed with
ADHD to the brains of those without. "The
first step was to find out if the brains are
different," said Dr. Giedd, coauthor of the
study, "and we've established that pretty
solidly now." Overall, brain size is about 5%
smaller in children with ADHD, mainly because
of the smaller size of two areas involved in
attention, the frontal cortex and the basal
ganglia. Other studies have since shown that
the basal ganglia of kids with ADHD are less
active during attention tests, and that
Ritalin, a stimulant, increases activity in
this part of the brain.
Still, MRI can't yet be used to diagnose this
or similar psychiatric conditions. On the
whole, brain scans of children with ADHD,
autism, and other conditions are different
from those of children without ADHD, but the
discrepancies are too small and too varied to
be used for individual diagnoses. "The truth
is, it is a very subtle finding," says Dr.
Castellanos. "I can't just look at an MRI and
say whether a child has ADHD."
If this combination of attention tests and MRI
proves effective, it may lead to a definitive
diagnosis, which would help everyone involved:
"When you are committing a child to long-term
medication, it's crucial to verify the source
of the illness or behavior," says Martin H.
Teicher, M.D., Ph.D., professor of psychiatry
at Harvard Medical School in Boston. "An MRI,
along with the behavioral test, gives parents
a much greater sense of confidence about using
drugs."
|
Is MRI Right for Your Child?
As promising as brain scanning is,
doctors caution that the field is still
in its infancy. "It'll probably be five
to 10 years before we can use MRI to
diagnose," says Dr. Giedd. So spending
the $800 to $2,000 it costs for a brain
scan will probably make no difference to
a child's diagnosis or treatment, says
Judith L. Rapoport, M.D., chief of the
child psychiatry branch at NIMH."But by
using MRI as a research tool, we lay the
groundwork for understanding what goes
wrong in brain development and how it
causes diseases," Dr. Rapoport says.
What's more, insurance companies will
not compensate for MRIs performed on
patients with neuropsychiatric
conditions. If brain imaging can
identify these disorders, they'll have
an impetus to cover MRIs. Earlier
diagnosis will allow for earlier
intervention and better prognoses --
"money in the bank for insurers,"
explains Dr. Teicher.
For now, diagnostic and treatment
options for children with
neurodevelopmental disorders are
limited. "But if we can understand what
affects brain development, then we can
get to the next step of intervention and
give practical advice to parents,
teachers, and children," says Dr. Giedd.
|
|
|
|
|
|
|